New claims management experience
Staying on top of claims is one of the most essential parts of the billing process. Designing an ideal solution for it isn’t straightforward. After updating various aspects along the way, we came to recognize the need for a distinctively new approach. Our team went to work. Aiming for maximum usability and day-to-day efficiency, they deeply analyzed your feedback and rethought our strategy.
Comprehensive DOS-level view
There are two primary places to access claims: the Billing > Bills screen and the “Bills” tab in the patient chart. One considers the universe of claims for convenient tracking; the other displays only the selected patient’s claims, offering more focused information. Both had their options reduced to a single View action (with the former also incorporating Cancel action):
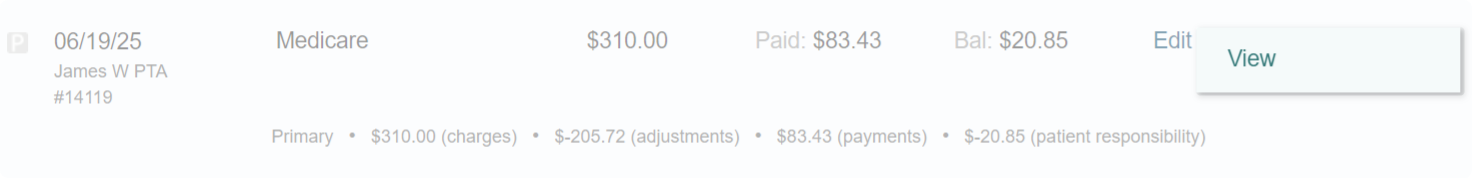
The view action will launch a fresh, modern interface (detailed below) that brings together everything you need to understand where your billing for a specific provider and date of service stands.
You’ll notice “claim” and “bill” are used interchangeably — they mean the same thing in therapyBOSS. We favor “bill” because it can refer to an insurance claim, a patient bill, or a referral source bill, all of which are seamlessly created and managed in therapyBOSS.
Toggling between dates of service
When accessing a claim containing several dates of service, therapyBOSS will present applicable information per date, allowing you to switch between them easily:
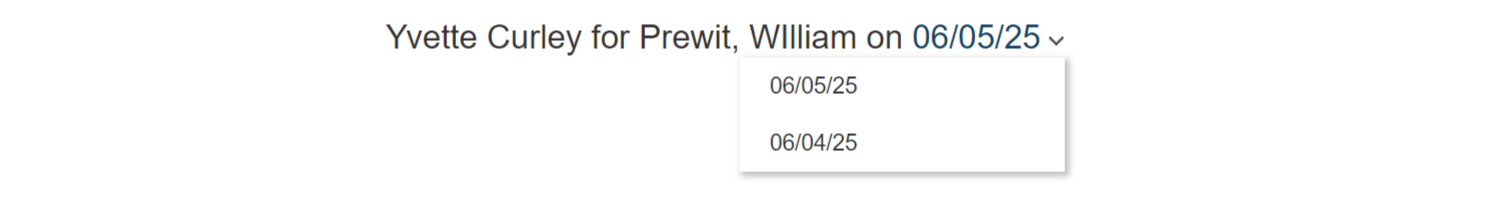
It’s a good idea to avoid different dates of service within a claim. That’s the new default in therapyBOSS. You can set it for existing payers by editing them under Settings and marking “Separate claim for different days“.
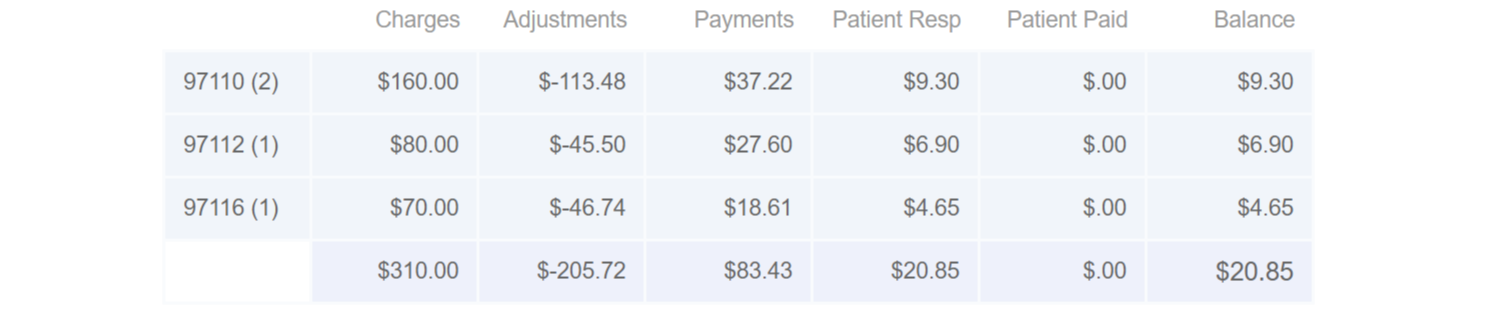
Summary of charges and payments
How much was billed, how much already paid, adjusted and the patient responsibility portion will be immediately evident, totaled per procedure code and accounting for all contributing payers:
Claim’s lifecycle at a glance
You’ll be able to figure out quickly where your claim is thanks to a unique, timeline-based presentation. This format, ideal for conveying a chain of events, fits perfectly here:
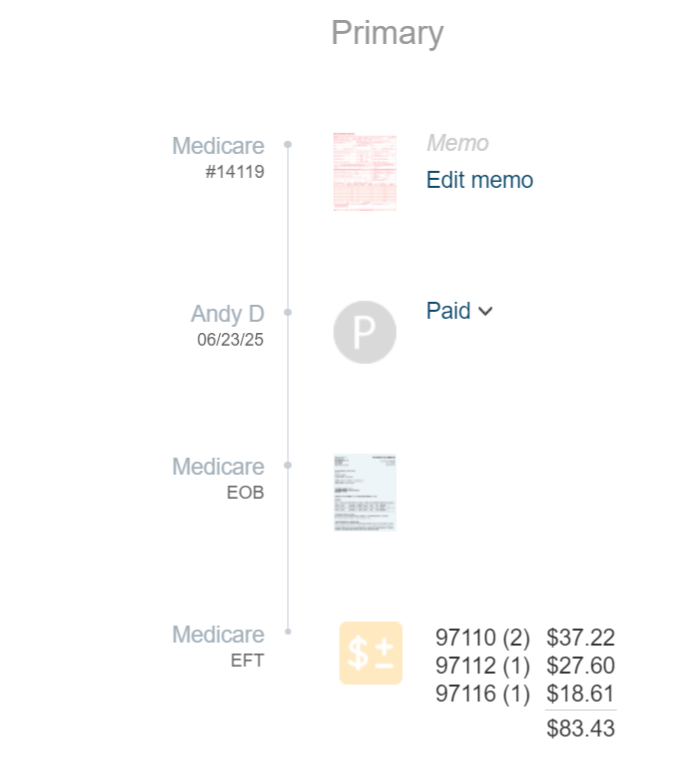
Timeline events, or points, will include the claim form, bill’s status, clearinghouse acknowledgement (if received), remittance/EOB (if obtained), and itemized payments and adjustments. Open them by pressing on the respective point. For example:
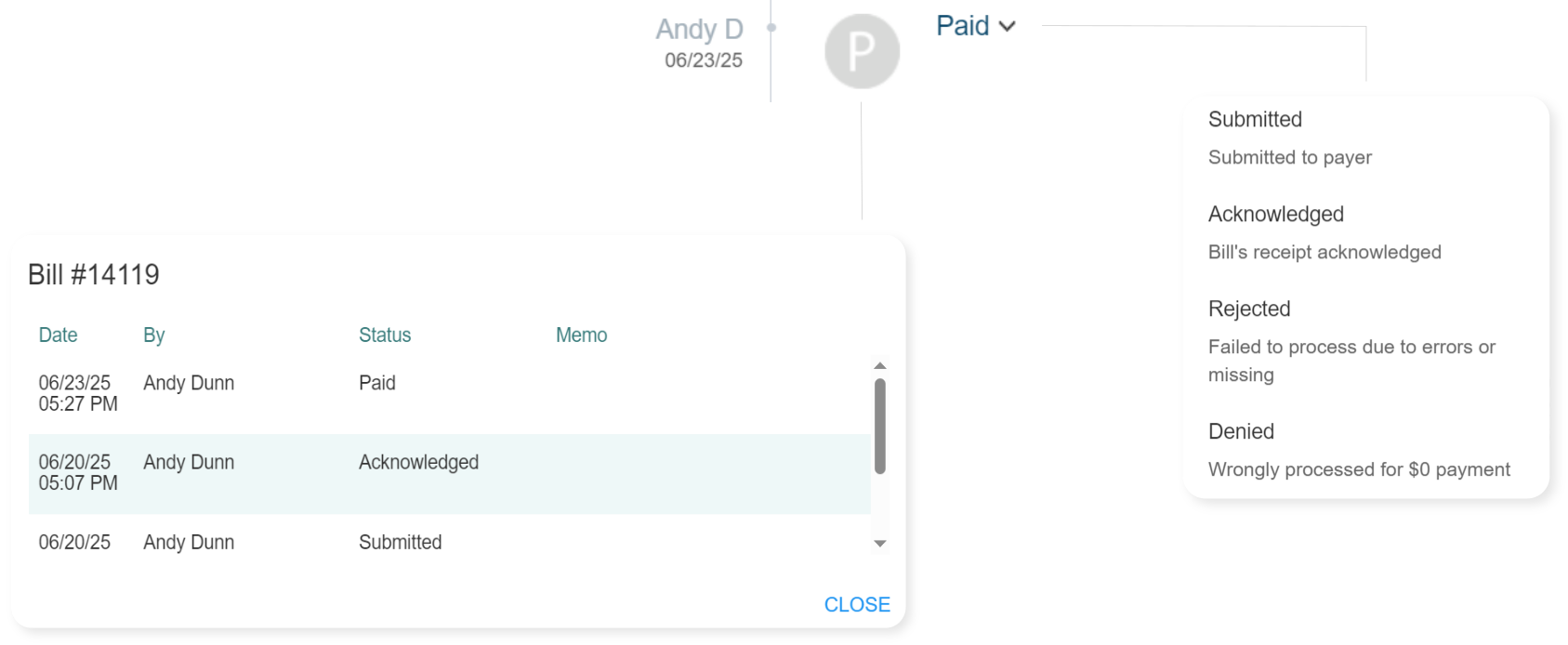
Every claim submission will have its own timeline. There would be two consecutive timelines, as an example, if some of the billed services get paid while others are denied and rebilled. Multiple timelines would also be there when claims are rejected, canceled in therapyBOSS, and resubmitted (though canceled claims will be hidden by default).
Streamlined claim form editing
Editing CMS-1500 or UB-04 will become less involved owing to an uncluttered presentation that cuts down to just one button:
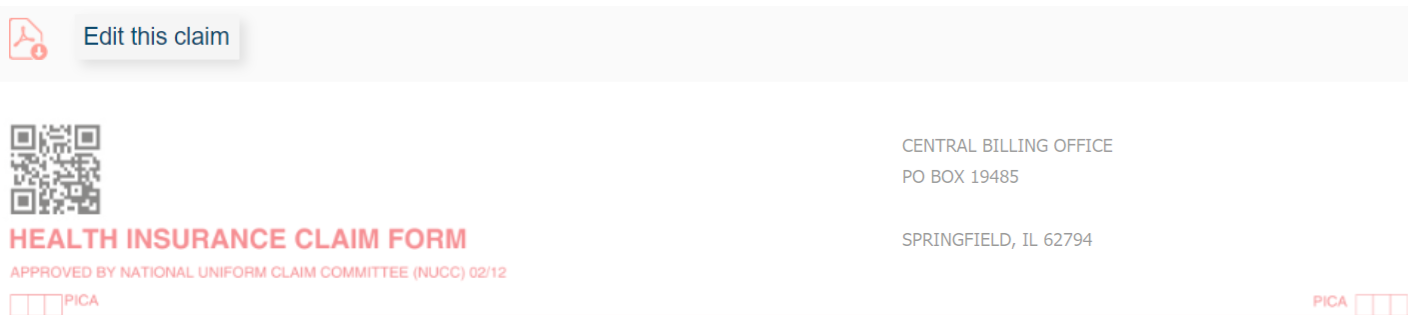
Activating edit mode will pull in any revisions found in the patient’s file, including changes to demographics, insurance, referring provider, and more.
Overhauled payment recording
This release brings a significant update to how payments are recorded. Use the corresponding timeline point to invoke a more robust framework for entering payments and adjustments:

You’ll continue to be able to record payments across multiple bills for a given payer:

The option to close a bill will appear when its status is Paid and the balance is 0:
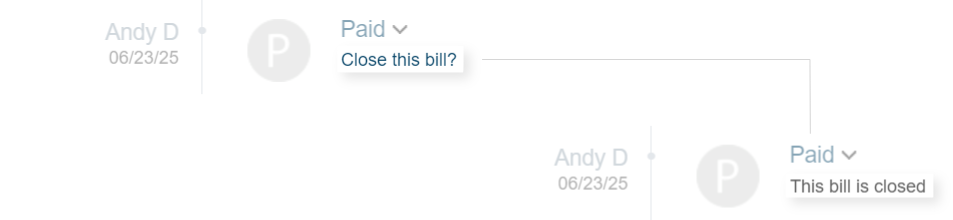
Certain actions, such as billing the next payer in sequence, will automatically close the bill when appropriate. FYI, closing bills is advisable because it removes them from “Open bills” under Billing > Bills, helping facilitate effective claim tracking.
PR counter-adjustments retired
We’re phasing out the special positive adjustment that was used to offset payer-applied PR adjustments to balance a bill.
You’ll no longer insert PR counter-adjustments. Any previously added will be ignored.
Claim’s actions one click away
Each timeline will end with actions that you could possibly want to execute in reference to the timeline’s claim:
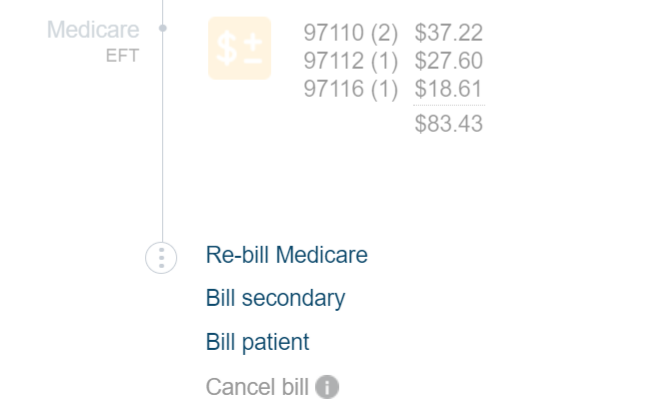
Actions that don’t apply will be disabled, with the reason clearly explained.
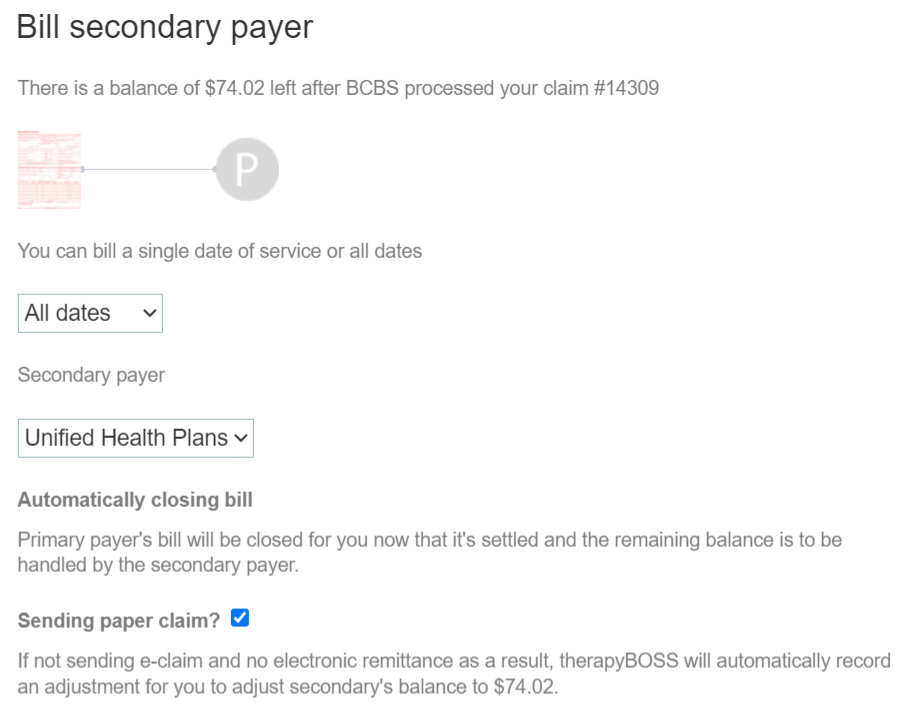
Billing secondary
Instant access to claim actions is complemented by an upgraded capability to bill secondary payers and patients. It will accomplish the same end result but with far greater usability:
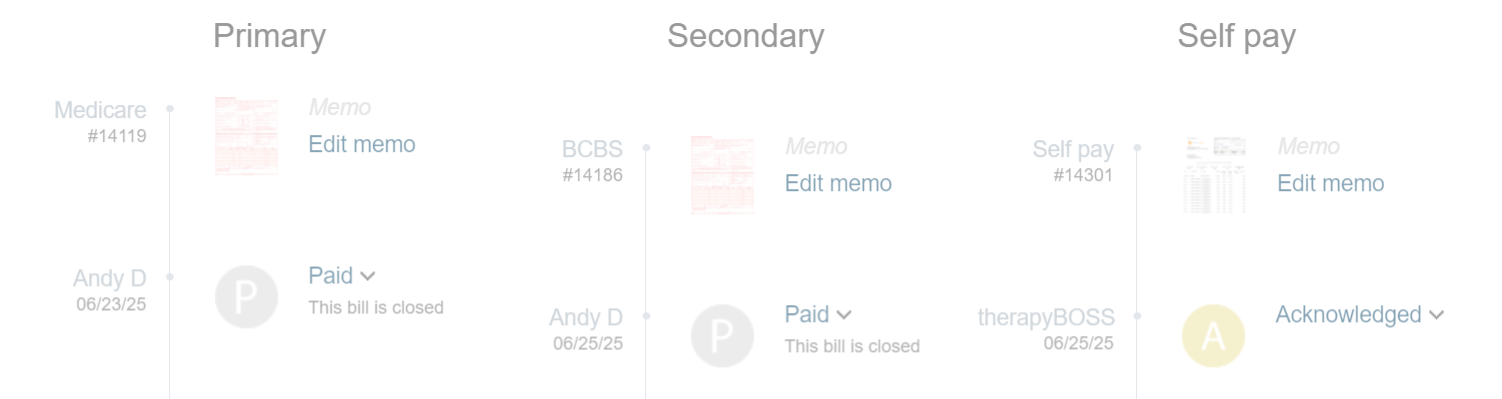
Participating payers unified
If both secondary and self pay are billed, separate timelines will be shown side-by-side, enabling you to quickly make sense of the full picture:
Redesigned remittances
The Remittances section has been largely rebuilt with intuitiveness and simplicity in mind. A cleaner layout and unambiguous controls will greet you when you navigate there:
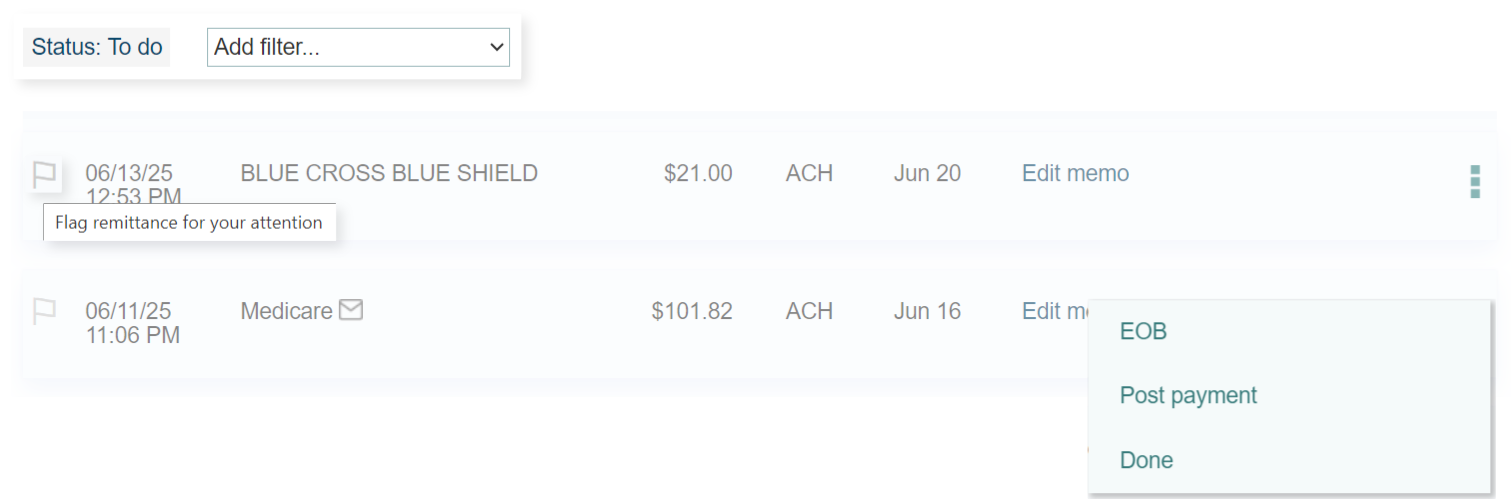
Major enhancements extend to payment posting and subsequent billing of additional payers:
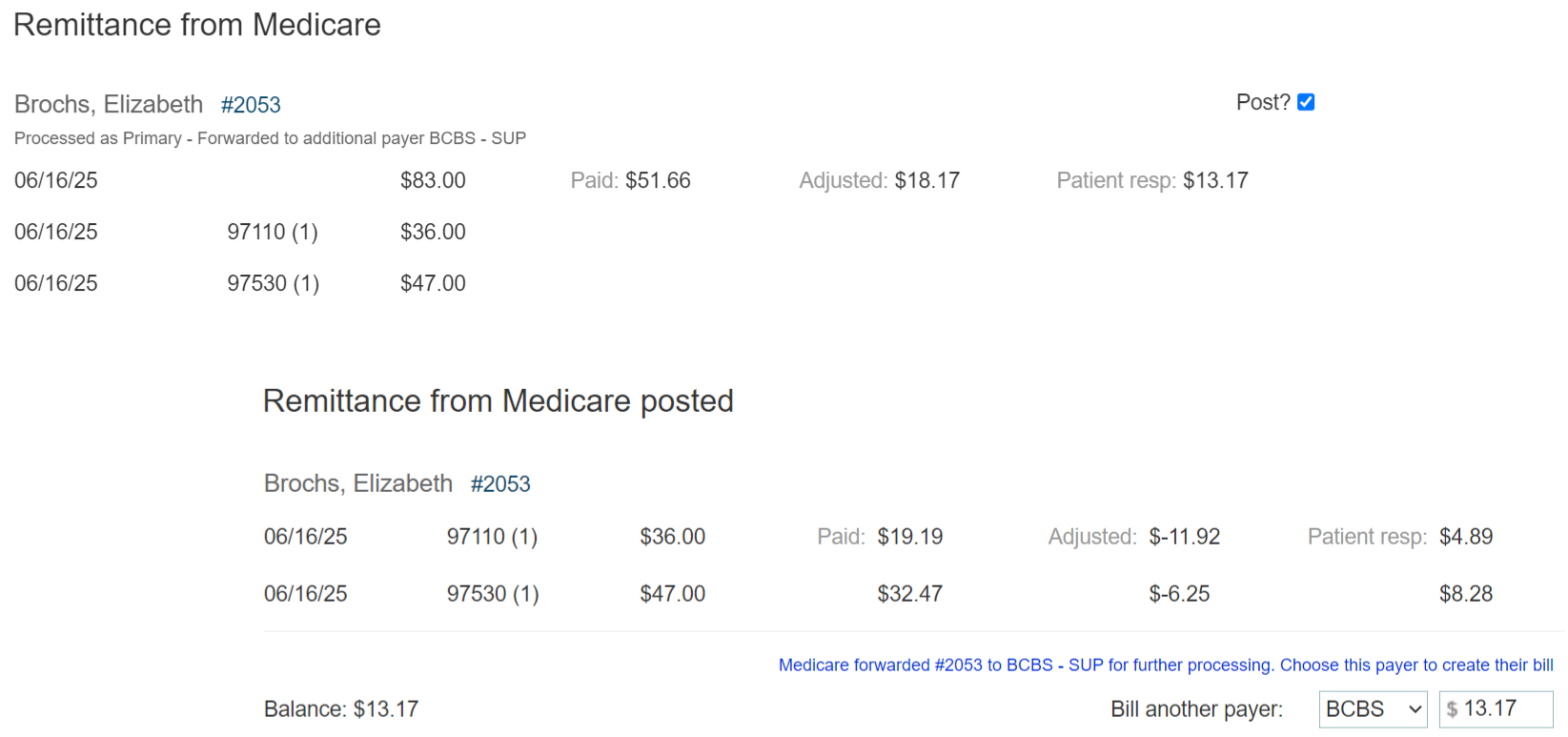
The entire flow is now extremely user-friendly and highly productive.
Clearinghouse reports refined
therapyBOSS has a built-in mechanism to download proprietary reports from your chosen clearinghouse. These reports are useful for spotting claim rejections. Their presentation was polished up to make working with them even simpler.
Patient’s view of bills improved
Bill information under the “Bills” tab in the patient chart was reordered slightly, achieving a more logical and clearer structure. Additionally, the shortcut to filter by date of service, previously only available when viewing “Per bill”, was added to “Per CPT/HCPCS” view as well.
